English
- Friday, 06 September 2019
- Hits: 5394
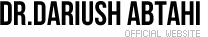
A pilonidal cyst is a fluid-filled sac. It forms beneath the skin near your tailbone, at the top of the crease of your buttocks. A pilonidal cyst that is not large or infected may not cause symptoms or problems.
If the cyst becomes irritated or infected, it may fill with pus. This causes pain and swelling (pilonidal abscess). An infected cyst may need to be treated with medicine, drained, or removed.

What are the causes?
The cause of a pilonidal cyst is not known. One cause may be a hair that grows into your skin (ingrown hair).
What increases the risk?
Pilonidal cysts are more common in boys and men. Risk factors include:
- Having lots of hair near the crease of the buttocks.
- Being overweight.
- Having a pilonidal dimple.
- Wearing tight clothing.
- Not bathing or showering frequently.
- Sitting for long periods of time.
What are the signs or symptoms?
Signs and symptoms of a pilonidal cyst may include:
- Redness.
- Pain and tenderness.
- Warmth.
- Swelling.
- Pus.
- Fever.
How is this diagnosed?
Your health care provider may diagnose a pilonidal cyst based on your symptoms and a physical exam. The health care provider may do a blood test to check for infection. If your cyst is draining pus, your health care provider may take a sample of the drainage to be tested at a laboratory.
How is this treated?
Surgery is the usual treatment for an infected pilonidal cyst. You may also have to take medicines before surgery. The type of surgery you have depends on the size and severity of the infected cyst. The different kinds of surgery include:
- Incision and drainage. This is a procedure to open and drain the cyst.
- Marsupialization. In this procedure, a large cyst or abscess may be opened and kept open by stitching the edges of the skin to the cyst walls.
- Cyst removal. This procedure involves opening the skin and removing all or part of the cyst.
Follow these instructions at home:
- Follow all of your surgeon’s instructions carefully if you had surgery.
- Take medicines only as directed by your health care provider.
- If you were prescribed an antibiotic medicine, finish it all even if you start to feel better.
- Keep the area around your pilonidal cyst clean and dry.
- Clean the area as directed by your health care provider. Pat the area dry with a clean towel. Do not rub it as this may cause bleeding.
- Remove hair from the area around the cyst as directed by your health care provider.
- Do not wear tight clothing or sit in one place for long periods of time.
- There are many different ways to close and cover an incision, including stitches, skin glue, and adhesive strips. Follow your health care provider's instructions on:
- Incision care.
- Bandage (dressing) changes and removal.
- Incision closure removal.
Contact a health care provider if:
- You have drainage, redness, swelling, or pain at the site of the cyst.
- You have a fever.
- Friday, 06 September 2019
- Hits: 3360
Cholecystitis is inflammation of the gallbladder. It is often called a gallbladder attack. The gallbladder is a pear-shaped organ that lies beneath the liver on the right side of the body. The gallbladder stores bile, which is a fluid that helps the body to digest fats. If bile builds up in your gallbladder, your gallbladder becomes inflamed. This condition may occur suddenly (be acute). Repeat episodes of acute cholecystitis or prolonged episodes may lead to a long-term (chronic) condition. Cholecystitis is serious and it requires treatment.
What are the causes?
The most common cause of this condition is gallstones. Gallstones can block the tube (duct) that carries bile out of your gallbladder. This causes bile to build up. Other causes of this condition include:
- Damage to the gallbladder due to a decrease in blood flow.
- Infections in the bile ducts.
- Scars or kinks in the bile ducts.
- Tumors in the liver, pancreas, or gallbladder.
What increases the risk?
This condition is more likely to develop in:
- People who have sickle cell disease.
- People who take birth control pills or use estrogen.
- People who have alcoholic liver disease.
- People who have liver cirrhosis.
- People who have their nutrition delivered through a vein (parenteral nutrition).
- People who do not eat or drink (do fasting) for a long period of time.
- People who are obese.
- People who have rapid weight loss.
- People who are pregnant.
- People who have increased triglyceride levels.
- People who have pancreatitis.
What are the signs or symptoms?
Symptoms of this condition include:
- Abdominal pain, especially in the upper right area of the abdomen.
- Abdominal tenderness or bloating.
- Nausea.
- Vomiting.
- Fever.
- Chills.
- Yellowing of the skin and the whites of the eyes (jaundice).
How is this diagnosed?
This condition is diagnosed with a medical history and physical exam. You may also have other tests, including:
- Imaging tests, such as:
- An ultrasound of the gallbladder.
- A CT scan of the abdomen.
- A gallbladder nuclear scan (HIDA scan). This scan allows your health care provider to see the bile moving from your liver to your gallbladder and to your small intestine.
- MRI.
- Blood tests, such as:
- A complete blood count, because the white blood cell count may be higher than normal.
- Liver function tests, because some levels may be higher than normal with certain types of gallstones.
How is this treated?
Treatment may include:
- Fasting for a certain amount of time.
- IV fluids.
- Medicine to treat pain or vomiting.
- Antibiotic medicine.
- Surgery to remove your gallbladder (cholecystectomy). This may happen immediately or at a later time.
Follow these instructions at home:
Home care will depend on your treatment. In general:
- Take over-the-counter and prescription medicines only as told by your health care provider.
- If you were prescribed an antibiotic medicine, take it as told by your health care provider. Do not stop taking the antibiotic even if you start to feel better.
- Follow instructions from your health care provider about what to eat or drink. When you are allowed to eat, avoid eating or drinking anything that triggers your symptoms.
- Keep all follow-up visits as told by your health care provider. This is important.
Contact a health care provider if:
- Your pain is not controlled with medicine.
- You have a fever.
Get help right away if:
- Your pain moves to another part of your abdomen or to your back.
- You continue to have symptoms or you develop new symptoms even with treatment.
- Friday, 06 September 2019
- Hits: 3653
The appendix is a finger-shaped tube that is attached to the large intestine. Appendicitis is inflammation of the appendix. Without treatment, appendicitis can cause the appendix to tear (rupture). A ruptured appendix can lead to a life-threatening infection. It can also lead to the formation of a painful collection of pus (abscess) in the appendix.

What are the causes?
This condition may be caused by a blockage in the appendix that leads to infection. The blockage can be due to:
- A ball of stool.
- Enlarged lymph glands.
In some cases, the cause may not be known.
What increases the risk?
This condition is more likely to develop in people who are 10–30 years of age.
What are the signs or symptoms?
Symptoms of this condition include:
- Pain around the belly button that moves toward the lower right abdomen. The pain can become more severe as time passes. It gets worse with coughing or sudden movements.
- Tenderness in the lower right abdomen.
- Nausea.
- Vomiting.
- Loss of appetite.
- Fever.
- Constipation.
- Diarrhea.
- Generally not feeling well.
How is this diagnosed?
This condition may be diagnosed with:
- A physical exam.
- Blood tests.
- Urine test.
To confirm the diagnosis, an ultrasound, MRI, or CT scan may be done.
How is this treated?
This condition is usually treated by taking out the appendix (appendectomy). There are two methods for doing an appendectomy:
- Open appendectomy. In this surgery, the appendix is removed through a large cut (incision) that is made in the lower right abdomen. This procedure may be recommended if:
- You have major scarring from a previous surgery.
- You have a bleeding disorder.
- You are pregnant and are near term.
- You have a condition that makes the laparoscopic procedure impossible, such as an advanced infection or a ruptured appendix.
- Laparoscopic appendectomy. In this surgery, the appendix is removed through small incisions. This procedure usually causes less pain and fewer problems than an open appendectomy. It also has a shorter recovery time.
If the appendix has ruptured and an abscess has formed, a drain may be placed into the abscess to remove fluid and antibiotic medicines may be given through an IV tube. The appendix may or may not need to be removed.
- Friday, 06 April 2018
- Hits: 3608
What Is Strabismus?
Strabismus is a condition in which the eyes don’t move in the same direction. They appear to point in different directions. One or both eyes may turn either in or out. Over time, the weaker eye becomes “lazier,” or less used, as the brain uses signals from the stronger eye.
Strabismus runs in some families. Treatment can correct this condition, but without early treatment, some vision may be lost.

What Causes Strabismus?
Strabismus has two causes. The first is a difference in strength of muscles around each eye. The second is a difference in each eye’s ability to focus. If either the muscle strength or focus of one eye is weaker, that eye may start to drift. Strabismus usually appears in early to middle childhood. It can also occur as early as at birth, but it’s hard to diagnose strabismus until 3 months of age, because at birth the eyes cannot focus well. Adults can also develop strabismus. In adults, a disease such as diabetes or stroke or injury to the eye can cause it.
What Are the Symptoms of Strabismus?
The main symptom is that the eyes seem to look in two different directions. Squinting, frequent eye rubbing, and tilting of the head are common. Double vision and vision in only one eye are other symptoms.
How Is Strabismus Diagnosed?
The health care provider will make a diagnosis by doing an eye examination. The examination may include looking through a set of prisms to find the differences between the eyes. The eye exam may also include a visual acuity test, examination of the retina, and a neurological examination. Your health care provider may suggest seeing an ophthalmologist (specialist in eye disorders). The specialist will also check nerves and muscles around the eyes. Then, decisions about whether surgery might fix the problem can be made.
Children should usually have their eyes examined every 1 to 4 months until the eyes are stable. After that, they may need examinations every 6 months until the age of 6 years. Annual examinations should follow until age 9 to 11.
How Is Strabismus Treated?
The goal of treatment is to make the weaker eye stronger. To do this, glasses or an eye patch over the stronger eye may be used. This forces the weaker eye to become stronger. The health care provider may suggest doing eye muscle exercises. Eye drops (atropine) may also be used in some cases. Sometimes, surgery is needed to balance the muscle strength between the two eyes.
DOs and DON’Ts in Managing Strabismus:
- DOwear the patch or eyeglasses, or both, given to you by your health care provider.
- DOcallyour health care provider if you get a fever or pain and redness in the eye after surgery.
- DON'Trun when you’re adjusting to wearing an eye patch. This will help prevent falls and injury.
Source: Clinicalkey.com
- Friday, 06 April 2018
- Hits: 4045
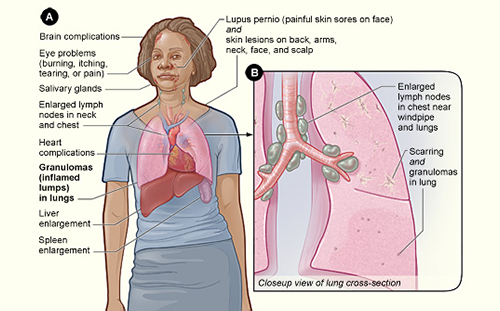
What Is Sarcoidosis?
Sarcoidosis is an illness that causes inflammation of many organs. It most often starts in the lungs or lymph nodes (glands). The illness affects both sexes and all ages but is more common in females between the ages of 20 and 40 years old.
What Causes Sarcoidosis?
The cause isn’t known. It is a granulomatous disease. Granuloma means a special kind of tissue inflammation seen with a microscope, and granulomatous means related to granuloma. Sarcoidosis isn’t contagious or hereditary, although the risk is increased if a close family member carries the diagnosis.
What Are the Symptoms of Sarcoidosis?
Some people have only one or two symptoms, but others have many. These may include shortness of breath, dry cough, joint aches and pain, chest pain, dry eyes, dry mouth, fever, large lymph glands, loss of appetite and weight, palpitations, chronic runny or stuffy nose, rash, and stiff or swollen joints. Other signs and symptoms are tiredness, vision changes, and tender red areas over the legs known as “erythema nodosum.” In complicated cases, eye inflammation, high blood calcium levels, liver and kidney problems, heart rhythm problems, and skin lesions may occur.
How Is Sarcoidosis Diagnosed?
The diagnosis is difficult, because people may not have symptoms, and other disorders can cause similar problems. The health care provider will do a physical examination and order a chest x-ray. The x-ray is often abnormal and the physical examination may be normal. The health care provider may want blood tests, breathing tests, computed tomography (CT), tissue biopsy, tuberculosis (TB) tests, and electrocardiography (ECG). If the health care provider needs a lung sample for diagnosis, a procedure called bronchoscopy will be done by a lung specialist (pulmonologist). The doctor puts a flexible tube through the nose into the lungs. If results are unclear, surgery to open the lungs and get a more extensive piece of tissue (open lung biopsy) may be done.
How Is Sarcoidosis Treated?
Many people get better without treatment, especially in earlier stages and people without symptoms. However, in people with severe symptoms, treatment may be needed for several weeks to years. Oral corticosteroids (anti-inflammatory steroids such as prednisone) usually help in 1 to 3 months, but close follow-up and dose changes are necessary. Prednisone is usually given for at least 6 to 12 months. Usually, the lowest dose to control sarcoidosis is used. Response to treatment is checked by watching for changes in symptoms, chest x-rays, breathing tests, and other abnormalities. Relapses may occur. For severe progressive disease not responding to prednisone, more powerful medications, such as methotrexate, azathioprine, or hydroxychloroquine, may be used.
DOs and DON’Ts in Managing Sarcoidosis:
- DOtell your health care provider about your medicines (prescription and over-the-counter).
- DOtell your health care provider if you’re pregnant.
- DOeat a low-salt diet if you take corticosteroids, to prevent fluid gain.
- DOhave your blood pressure checked and blood tested for diabetes while taking corticosteroids.
- DOget a flu shot each fall.
- DOget vaccinated for pneumococcal pneumonia.
- DOcall your health care provider if you’re very thirsty, urinate a lot, or have weight changes. It could indicate a very high sugar level from prednisone.
- DOcall your health care provider if you cough discolored sputum or blood.
- DOcall your health care provider if you have fever, chills, vision changes, chest pain, or palpitations.
- DOcall your health care provider if your symptoms don’t get better or get worse.
- DON’Tstop taking your medicine or change your dosage because you feel better, unless your health care provider tells you to.
- DON’Tsmoke. Smoking makes symptoms worse.
- DON’Tget too much direct sun exposure. It will make any skin rash from sarcoidosis worse.
source: clinicalkey.com
- Friday, 06 April 2018
- Hits: 5409
What Is Osteoporosis?
Osteoporosis is the continuing thinning and loss of density in bones (bone mass), which makes bones more brittle, fragile, and likely to break after minor trauma. Loss of height and back pain are common. Women are at special risk for osteoporosis after their menstrual periods end (menopause), because quicker bone loss occurs after reduced production of the hormone estrogen. Estrogen blocks a protein that weakens bones.
Osteoporosis is a silent disease, and it may not be evident until a bone breaks.

What Causes Osteoporosis?
Normal bone formation needs the minerals calcium and phosphate. If the body does not get enough calcium from the diet, bone production and bone tissues may suffer.
The main causes of osteoporosis include aging, which leads to a drop in estrogen in women at menopause and a drop in testosterone (a male hormone) in men. Other causes are being underweight, lifestyle habits (being sedentary or inactive), alcohol use, cigarette smoking, eating disorders, taking certain drugs, some chronic diseases, and long-term bed rest or immobilization.
What Are the Symptoms of Osteoporosis?
No symptoms may be obvious early in the disease, but in time, low back and neck pain, stooped posture, and gradual loss of height may be seen. In other cases the first sign is a fracture (ribs, wrists, or hips). Bones (vertebrae) in the spine may collapse (become flattened or compressed) and break, which is the most common fracture. Hip fractures can cause the greatest disability.
How Is Osteoporosis Diagnosed?
The physician will take a medical history and do a physical examination to look for age-related signs of a deformed spine. Laboratory tests can measure calcium and vitamin D levels. An x-ray examination called DEXA can measure bone density at important places, such as the spine and the hip. Screening for osteoporosis may be recommended for all women after menopause and for men with risk factors such as long-term use of corticosteroids such as prednisone, which predisposes to osteoporosis.
How Is Osteoporosis Treated?
Lifestyle changes may help reduce fracture risk. Such changes include doing regular weight-bearing and muscle-strengthening exercises, stopping smoking, limiting alcohol intake, and getting enough calcium (at least 1,200 mg/day) and vitamin D (at least 800 IU/day) in the diet. Treatments focus on slowing down or stopping bone loss and on preventing bone fractures by minimizing the risk of falls.
Different drugs, including bisphosphonates such as alendronate, taken weekly may be prescribed in addition to adequate supplementation of calcium and vitamin D. Several other medications are also available.
DOs and DON’Ts in Managing Osteoporosis:
- DOregular weight-bearing and muscle-strengthening exercises as suggested by your health care provider.
- DOmake sure you get enough calcium and vitamin D. Eat a healthy diet that is rich in calcium-containing foods, such as dairy products, fish, beans, and green leafy vegetables.
- DOtake your medicines as prescribed.
- DOdiscuss screening for osteoporosis with your health care provider.
- DON’Tsmoke.
- DON’Tdrink alcohol in excess.
sourse: clinicalkey.com